Orchid's team of genetic experts has developed a genetic risk score (GRS) for class III obesity.
Written by Orchid Team
Orchid has developed advanced genetic risk scores (GRS) for a variety of diseases. Here we present our data on our GRS of class III obesity.
Class III Obesity
Class III obesity is defined as a body mass index (BMI) of at least 40 kg/m² and is the most severe category of obesity based on standard BMI classification. It is associated with markedly increased morbidity and mortality, including substantially elevated risks of type 2 diabetes, cardiovascular disease, sleep apnoea, certain cancers, impaired physical function, and reduced quality of life. Environmental risk factors include living in settings with abundant energy-dense foods and limited opportunities for physical activity. Excessive weight gain by either the mother during pregnancy or by the child after birth are also risk factors.[1]
Genetic Risk Score
Class III obesity is shaped by both environmental and genetic factors. Monogenic testing is not available because no single gene causes the condition. Genetic risk scores (GRS), which combine the small effects of many variants into a single score, are currently the only way to estimate genetic risk. Although not diagnostic, a GRS can indicate how likely an individual is to develop the disease.
Orchid’s class III obesity GRS was trained following current industry standards.[2][3] The GRS was constructed using the SBayesRC algorithm trained on publicly available FinnGen and Million Veterans Program summary statistics.[4][5] The summary statistics include 277,884 cases and 799,863 controls.[6] The resulting GRS contains over a million variants.
Risk predictions are adjusted to each individual’s ancestry, with predictive power decaying as genetic distance from the predominately European training data increases.[7] Orchid considers a GRS meaningfully predictive if individuals at roughly the 97.7th percentile have an odds ratio (OR) of 2. The class III obesity GRS meets this criteria for all common ancestry groups.
Clinical Impact and Prevalence
Obesity is highly prevalent worldwide, with the WHO estimating that >2.1 billion adults were overweight or obese in 2014.[1] In the United States, the CDC estimates that 9.2% of adults suffered from class III obesity between 2017 and 2020.[8]
Treatment of obesity focuses first on lifestyle changes such as improving diet and increasing physical activity. If these lower-risk approaches are not enough, medications can be used as add-ons to diet and exercise for selected patients. Bariatric surgery is an option for severe obesity that can produce substantial, longer-term weight loss but requires careful risk–benefit consideration.[1]
Performant Risk Stratification
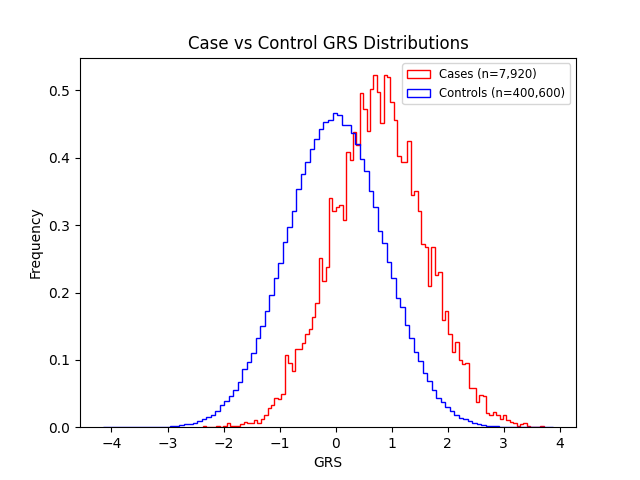
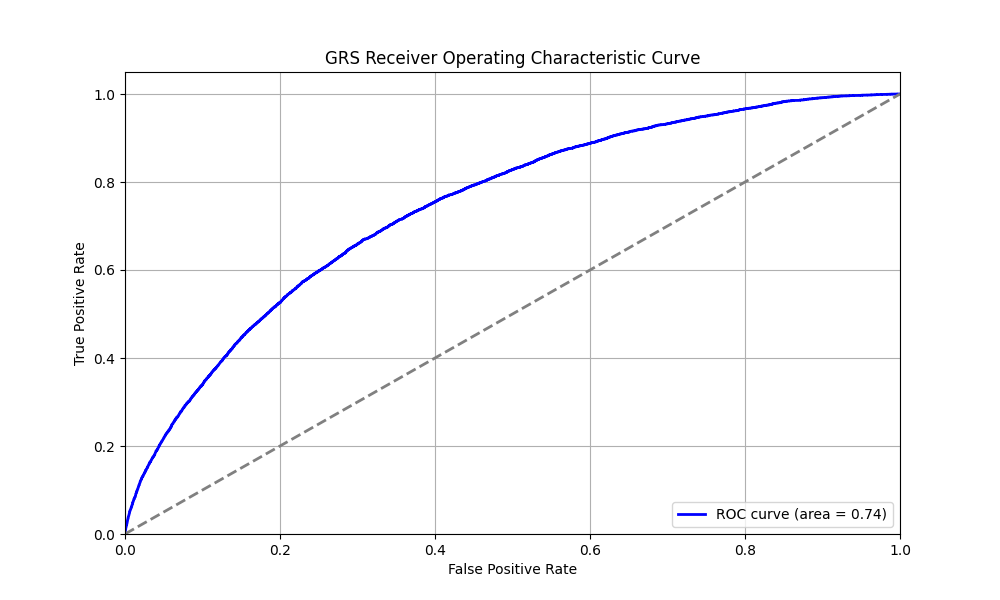
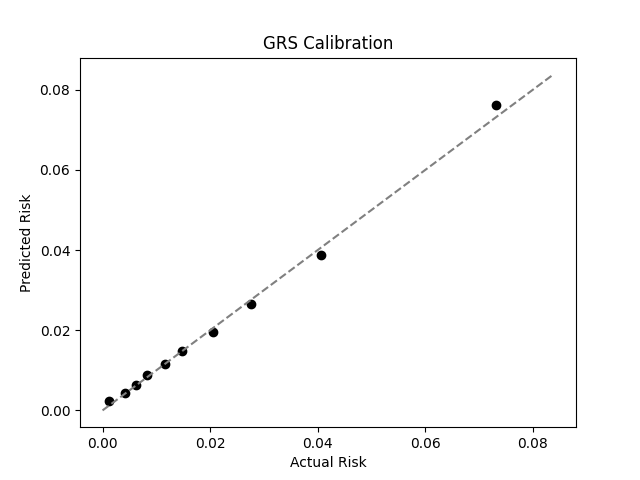
We evaluated the predictive performance of Orchid’s class III obesity GRS using the UK Biobank (UKB), a research database of roughly 500,000 genotyped individuals from the United Kingdom. We restricted the analysis to participants of British ancestry and defined class III obesity as a BMI of at least 40, yielding 7,920 cases and 400,600 controls (1.9% prevalence). We then grouped individuals by GRS percentile and compared the observed disease prevalence within each group to our model’s predictions (Figure 1). For additional technical details, see the Supplementary Data.
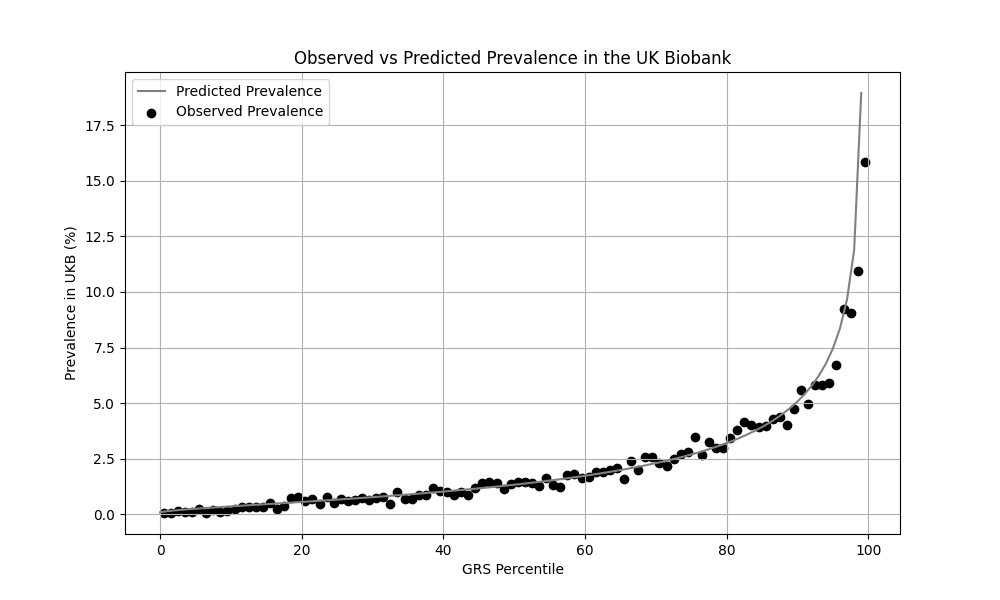
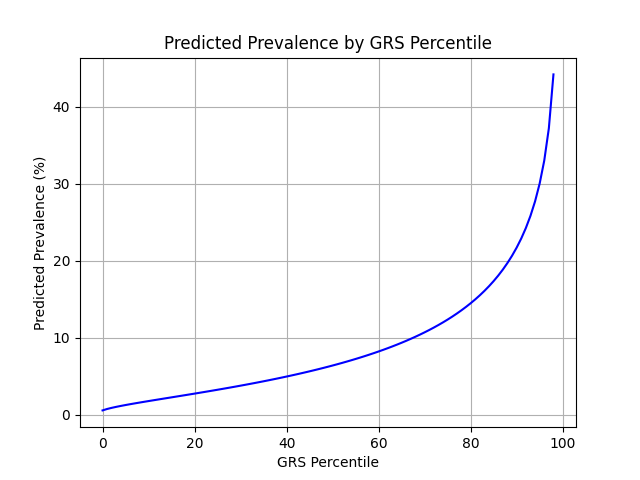
UKB participants tend to be healthier than the general population, which leads to lower observed disease prevalence.[9] The CDC estimates a 9.2% prevalence within the U.S., much higher than the prevalence in the UKB.[8] We adjust our model so that its average predicted risk aligns with this estimate (see Figure 2).[10] People at the tail end of the GRS distribution were at an elevated risk compared to the mean (see Table 3), with adults in the 99th percentile 4.8x more likely to develop class III obesity than average (44.2% vs 9.2%).
References
1. González-Muniesa P, Martínez-González MA, Hu F, et al. Obesity. Nat Rev Dis Primers. 2017;3:17034. doi:10.1038/nrdp.2017.34.
2. Moore S, Davidson I, Anomaly J, et al. Development and validation of polygenic scores for within-family prediction of disease risks. medRxiv. 2025. doi:10.1101/2025.08.06.25333145.
3. Cordogan S, Starr DB, Treff NR, et al. Within- and between-family validation of nine polygenic risk scores developed in 1.5 million individuals: implications for IVF, embryo selection, and reduction in lifetime disease risk. medRxiv. 2025. doi:10.1101/2025.10.24.25338613.
4. Zheng, Z., Liu, S., Sidorenko, J. et al. Leveraging functional genomic annotations and genome coverage to improve polygenic prediction of complex traits within and between ancestries. Nat Genet 56, 767–777 (2024). https://doi.org/10.1038/s41588-024-01704-y
5. FinnGen. FinnGen+MVP+UKBB Summary Statistics. Available at: https://mvp-ukbb.finngen.fi/about. Accessed 2025-12-05.
6. FinnGen. FinnGen+MVP+UKBB Phenotypes. Available at: https://mvp-ukbb.finngen.fi. Accessed 2025-12-15.
7. Privé, Florian et al. “Portability of 245 polygenic scores when derived from the UK Biobank and applied to 9 ancestry groups from the same cohort.” American journal of human genetics vol. 109,1 (2022): 12-23. doi:10.1016/j.ajhg.2021.11.008
8. Centers for Disease Control and Prevention. Adult Obesity Facts. Available at: https://www.cdc.gov/obesity/adult-obesity-facts/. Accessed 2025-12-17.
9. Fry A, Littlejohns TJ, Sudlow C, et al. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–1034. doi:10.1093/aje/kwx246
10. Chatterjee N, Shi J, García-Closas M et al. Developing and evaluating polygenic risk prediction models for stratified disease prevention. Nat Rev Genet. 2016;17:392–406. doi:10.1038/nrg.2016.27
Supplementary Figures
Acknowledgements
This research has been conducted using the UK Biobank Resource under Application Number 80545.